This morning, the Department of Health and Social Care (DHSC) released a new 10 Year Health Plan for England.
Commenting on the plan, the Prime Minister, Keir Starmer, said the health system the Labour Government inherited was in crisis. “That ends now…it’s reform or die”.
The new health plan is set to be at the forefront of a new model of care, creating a system fit for the future. This is guided by three core shifts: hospital to community, analogue to digital and sickness to prevention.
In this article, we delve into the government’s groundbreaking new health plan, dissecting its core principles with insights from official press releases and presenting key data that underpins these transformative changes.
Data is key in informing government decisions and policy, and the NHS health plan is no different. Throughout the policy paper, the DHSC references NHS staff survey data, figures from the ONS, data on smoking trends, among others, to support its policy points.
Additional statistical releases highlighted throughout this blog give further context to the need for change.
Hospital to community
On the 2nd of July, the DHSC announced its plans to bring more easily accessible care to neighbourhoods, in an attempt to move care from hospitals to community services.
Neighbourhood Health Services
The government seeks to bring the NHS closer to home through three key measures:
-
- Creation of Neighbourhood Health Services, bringing diagnostics, mental health, post-op, rehab and nursing to people’s doorsteps
- Housing services under one roof – Neighbourhood Health Centres (NHC) – to be open at evenings and weekends
- Rebuilding the NHS to train thousands more family doctors, transform hospital outpatient appointments, and provide personalised care plans for complex needs.
The Neighbourhood Health Service will embody a new preventative principle: care should happen as locally as it can, digitally by default, in a patient’s home if possible, in a NHC when needed, and in a hospital if necessary. This way, the plans come as a way of freeing up hospital resources and tackling NHS waiting times.
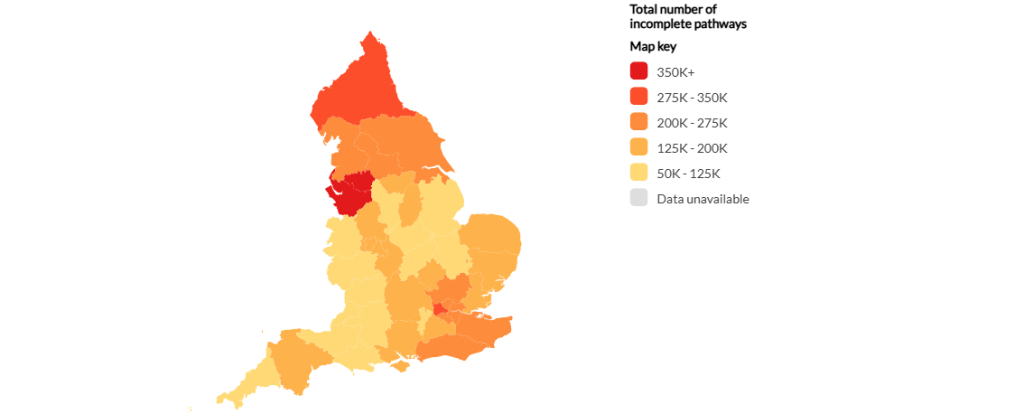
According to the latest NHS waiting times figures, all ICBs in England continue to significantly miss targets, despite incomplete pathways falling by 2.4% over the year.
Polimapper’s visualisation shows that, in the Mid and South Essex Integrated Care Board, less than 50% of open pathways were completed within the 18 week target. Click here to launch our waiting times visualisation.
Rebuilding NHS in working-class communities
A key part of the health plan is also the commitment to tackling health inequalities by improving care in working-class communities and coastal areas. To achieve this, changes encompass investing in moving critical resources to regions that most need them and changing how GP funding is distributed.
According to the Index of Multiple Deprivations rank, Blackpool is the most deprived area in the country, whilst Hart is the least. Blackpool also sees one of the lowest rates of people who report having a very good health status, according to the 2021 census, and one of the highest rates of physically inactive adults. In Hart, these figures reveal the opposite picture.
Health inequalities in England go hand in hand with deprivation and wellbeing measures. Learn more here.
Analogue to digital
The NHS is set to make a big move to digital by leveraging key technology to ensure rapid access for those in generally good health, free up physical access for those with complex needs, and help ensure the NHS’s financial sustainability.
NHS App overhaul
The government is set to introduce an upgraded NHS App to tackle health inequalities and give patients access to better care. This tool will democratize healthcare, empowering patients with greater choice and control over their own care, guided by insights on satisfaction, waiting times, and healthcare outcomes.
According to data from the Health Insight Survey, conducted in April 2025, over 18% of people in the Derby and Derbyshire Integrated Care Board had a poor experience in GP practices in the month.
Additionally, Polimapper’s visualisation shows that in the NHS Sussex Integrated Care Board over 50% of people were dissatisfied with the communication of NHS waiting times.
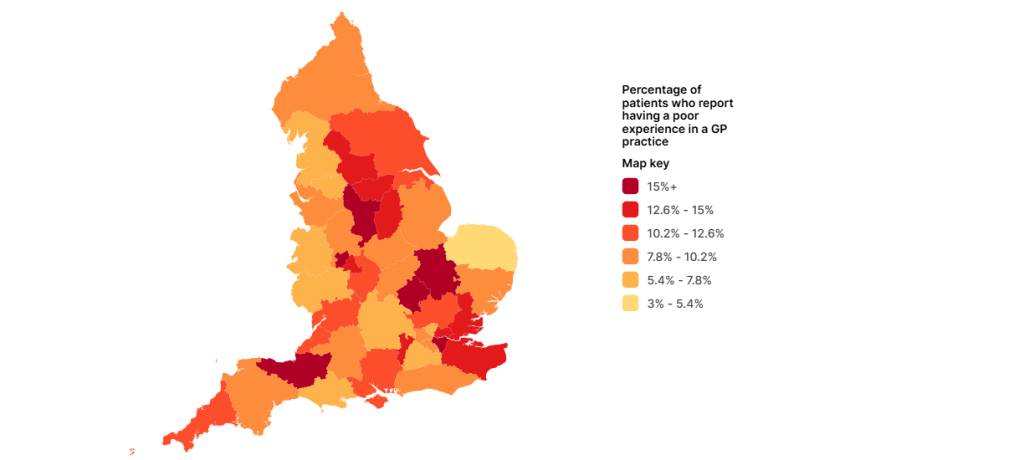
The introduction of greater control over one’s healthcare has the potential of streamlining service delivery and improving satisfaction rates in the future.
Digital change through AI
The DHSC revealed that AI will be at the forefront of the digital change brought by the 10 year plan. Pioneering AI technology is being developed to scan NHS systems to flag safety issues in real time and trigger crucial inspections earlier.
The Health and Social Care Secretary, Wes Streeting, has pledged to overhaul health and care regulation, root out poor performance and guarantee safe quality care through AI advances.
The tech work is already well underway, as a new maternity outcomes signal system will launch across NHS trusts from November. This will use near real-time data to flag higher than expected rates of still-birth, neonatal death, and brain injury.
Despite a fall in child mortality rates within the 20 years to 2023, rates significantly increased to 11.2 per 100,000 between 2021 and 2023, figures from the Office for Health Improvement and Disparities show. In Tameside mortality rates amongst 1 to 17 year olds were as high as 24.1 per 100,000.
Sickness to prevention
With its 10 year health plan, the Labour Government aims to shift priorities from sickness to prevention. The overall goal is to tackle the healthy life expectancy gap between the richest and poorest regions. Greater prevention will not only boost help but also ensure the future sustainability of the NHS.
The move from sickness to prevention will see the following measures:
- Further regulate Tobacco and Vapes for young people through the Tobacco and Vapes Bill and tackle harmful alcohol consumption by introducing new standards for alcohol labelling
- Tackle obesity by restricting junk food advertising targeted at children and harnessing recent breakthroughs in weight loss medication
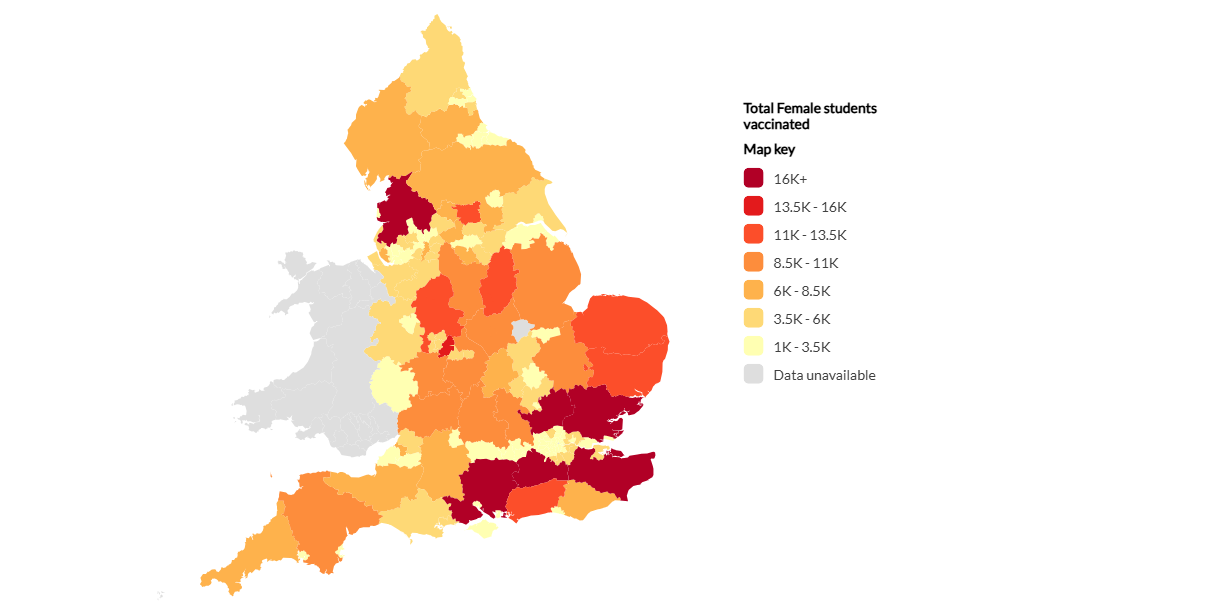
- Create a new genomics population health service to enable early identification and intervention for individuals at high risk of common diseases and increase uptake of HPV vaccinations.
Data from the Office for Health Improvement and Disparities shows that, in 2023/24, infectious diseases were the primary reason for over 20% of hospital bed usage in England. This had an annual cost of nearly £6bn to the NHS.
Additionally the latest HPV vaccination in England statistics show that, in the academic year 2023/24, the vaccination coverage dropped by 1.6% compared to the previous year among year 9 females, and 1.2% among year 9 males. Explore local area figures here.
Cautious optimism in early reactions
Despite the government’s optimistic outlook, various organisations fear promises brought by the plan may be unachievable and prioritise the institution over public health outcomes.
Dr Jennifer Dixon DBE, chief executive of The Health Foundation: “From what we’ve seen so far, the broad ambitions of the 10-year health plan […] are the right direction for the NHS.”
“However, these ambitions have appeared in NHS plans for decades, so the question now is whether they will be backed up by the concrete policy changes and investment needed to turn them from rhetoric to reality. A clear delivery plan backed up by the right leadership and support will be needed. Otherwise, the critical benefits of AI and technology may not be realised.”
“While we await the detail, the risk is that it is a plan for the NHS rather than a plan for health. To tackle the UK’s stalling health, and for the NHS to remain sustainable, a comprehensive cross-government strategy is needed for rebuilding the nation’s health […].”
Rachel Power, chief executive of the Patients Association: “For too long, the NHS has made decisions about patients, not in partnership with them. The 10 Year Health Plan signals a turning point but the proof will be in how patients shape its delivery.”
“But the plan alone won’t change lives. Turning this vision into reality starts now, and it must embed a culture of listening to patients, where they are involved at every stage, not sidelined or treated as an afterthought.
“[…] with nearly one in four still facing barriers to digital access, we must ensure that innovation doesn’t come at the cost of inclusion. If the NHS App is to become the digital front door, there must always be a real-world, accessible front door as well, with face-to-face or telephone options in place for those who need or want them. True progress means making the system work for everyone.”
Matthew Taylor, chief executive of the NHS Confederation: “The ten-year health plan is a landmark moment for both the NHS and wider health and care system. We welcome its bold ambitions, and our members stand ready to work in partnership with the government and NHS England to make the vital reforms needed to put the NHS on a long-term sustainable footing. The reality is that without the radical action outlined in the plan, the NHS as a universal service is in unprecedented danger.”
“A key part of making sure this plan is successful will be resetting the relationship between the NHS and the public so that local communities are placed at the heart of these reforms and people are supported to be active agents in their own health and wellbeing.

